What is blastocyst transfer?
Blastocyst transfer is a technique used during in vitro fertilization (IVF) in which an embryo is allowed to develop in a laboratory for five to six days after fertilization until it reaches a stage called the blastocyst. The blastocyst is then transferred into the uterus of the intended mother in the hope of achieving a successful pregnancy. The technique allows for the selection of the most viable embryos for transfer, potentially increasing the chances of pregnancy success.
Blastocyst transfers can be performed using fresh or frozen embryos depending on the individual patient's needs and circumstances. Couples who choose this option may undergo hormone therapy beforehand to prepare their body for embryo implantation.
How is blastocyst transfer different from traditional IVF?
- Blastocyst transfer is an advanced form of in vitro fertilization (IVF) since it involves transferring embryos to the uterus at a later stage of development.
- In traditional IVF, embryos are typically transferred to the uterus three days after fertilization. However, with blastocyst transfer, embryos are allowed to develop for five or six days before being implanted.
- Since only high-quality embryos can survive until day five or six of development, blastocyst transfer may increase the chances of successful implantation and pregnancy.
- Additionally, it may reduce multiple pregnancies since fewer quality blastocysts are transferred than in traditional IVF.
Anatomy
What is the structure of a blastocyst?
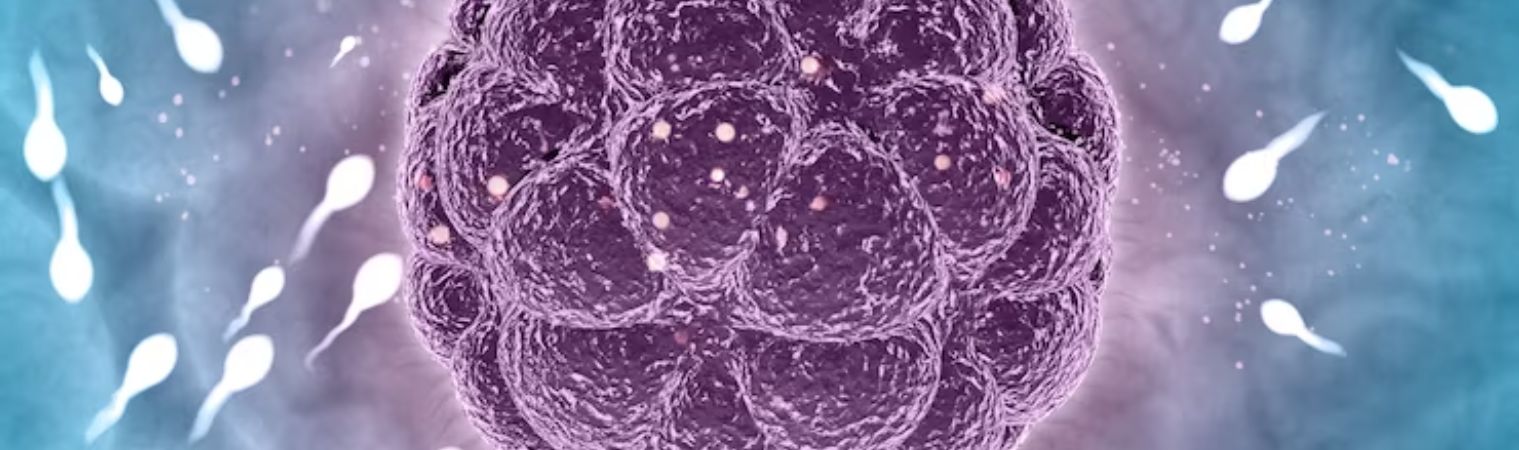
- The term 'blastocyst' refers to an embryo that has developed over several days.
- Currently, there is no way to get a cell count in late-stage preimplantation embryos without using invasive methods. However, data shows that there are about 100 cells in a 5-day-old embryo.
- Blastocysts have two distinct parts:
- the inner cell mass, which will eventually become the fetus, and
- the outer layer of cells called trophoblasts which will form into the placenta.
Why is blastocyst transfer performed?
Blastocyst transfer is performed because it has proven to be successful in increasing pregnancy rates while minimizing the risk of complications during pregnancy. This technique offers hope to many individuals or couples who have been unsuccessful with other fertility treatments and wish to start a family.
- It allows increased chances of conception for those struggling with infertility.
- It allows embryos to develop in vitro for longer, resulting in higher-quality embryos being transferred into the uterus.
- It allows the selection of the best embryos that have achieved genomic activation and have good implantation potential.
- It allows a higher chance of synchronization of the uterine endometrium and the embryos
Note: The blastocyst is an early-stage embryo that has activated its own genes, which determines its unique characteristics. This process is called "genomic activation," and it marks the point where a new and distinct individual is formed.
When do you need a blastocyst transfer?
- Blastocyst transfer is typically recommended for couples who have struggled with infertility and have undergone one or more failed rounds of in vitro fertilization (IVF).
- It's also a viable option for women over the age of 35, as well as those who have been diagnosed with certain medical conditions that affect fertility.
- If you've had multiple unsuccessful IVF cycles, your doctor may suggest trying blastocyst transfer. This technique involves waiting until day five or six after fertilization to transfer embryos into the uterus. By this point, only the strongest and healthiest embryos will have developed into blastocysts, increasing the chances of implantation and successful pregnancy.
- In addition to improving success rates for those struggling with infertility, blastocyst transfer can also be beneficial for couples undergoing genetic testing prior to IVF. Embryos that are found to be free of genetic abnormalities can then be transferred at the blastocyst stage in order to increase their chance of implantation.
If you're struggling with fertility issues or looking to maximize your chances of success during IVF treatment, it's worth discussing whether blastocyst transfer could be right for you.
Risks and Benefits
What are the risks and disadvantages of blastocyst transfer?
As with any medical procedure, there are risks and disadvantages associated with blastocyst transfer.
- Multiple pregnancies: One risk is the potential for multiple pregnancies if more than one embryo is transferred. This may heighten the chances of complications throughout pregnancy and childbirth. The risk of multiple pregnancies could be reduced by resorting to single blastocyst transfer.
- Chances of failure: Another disadvantage is that not all embryos will develop into blastocysts, which means fewer embryos may be available for transfer. Additionally, transferring a blastocyst does not guarantee a successful pregnancy or implantation.
- Infection: There is also a small risk of infection or bleeding from the insertion of the catheter during the transfer procedure. However, these risks are rare and can often be avoided through proper sterile techniques.
- Emotional stress: Some individuals may experience emotional stress or anxiety throughout the process of assisted reproduction and fertility treatments in general. It's important to seek support from healthcare professionals as well as loved ones during this time.
While there are certain risks involved in blastocyst transfer, it remains an effective option for many individuals struggling with infertility who wish to pursue parenthood through assisted reproductive technology.
What is the success rate of blastocyst transfer?
The success rate of blastocyst transfer depends on several factors, including the age and health of the woman, the quality of the embryos, and other individual circumstances.
- In general, studies have shown that blastocyst transfers tend to have higher success rates than earlier-stage embryo transfers.
- Women who underwent a blastocyst transfer had a clinical pregnancy rate of 62%, compared to a rate of 29% for those who underwent cleavage-stage embryo transfer.
- However, it's important to keep in mind that these statistics are just averages, and every individual case is different. Your doctor can give you more personalized information about your chances of success with a blastocyst transfer based on your specific situation.
- In addition to age and embryo quality, other factors that can affect the success rate of blastocyst transfer include underlying medical conditions (such as endometriosis or polycystic ovary syndrome), lifestyle factors like smoking or obesity, and previous fertility treatments or miscarriages.
There are some risks and disadvantages associated with this procedure such as multiple pregnancies, but they are minimal compared to the benefits it can offer couples trying to conceive.
Comparison of blastocyst stage transfer and cleavage stage embryo transfer?
Blastocyst stage transfer and cleavage stage embryo transfer are two common methods used in IVF. Understanding the differences between blastocyst stage transfer and cleavage stage embryo transfer can help you make an informed decision about which method is best suited for your specific needs during your journey towards parenthood.
- Cleavage-stage embryo transfer typically takes place on day three of fertilization, while blastocyst-stage transfer occurs on day five or six.
- One benefit of blastocyst transfer is that it allows for a better selection of embryos. By waiting until the blastocyst stage, embryologists can better determine which embryos have developed normally and are more likely to result in a successful pregnancy.
- On the other hand, cleavage-stage embryo transfers may be preferred for patients who produce fewer eggs during the IVF process. This method allows for earlier implantation and may increase the chances of success with limited numbers of embryos.
It's important to note that both methods have their own unique advantages and disadvantages, such as cost differences and potential risks associated with multiple pregnancies. Ultimately, choosing between these two methods will depend on individual circumstances and should be discussed thoroughly with a healthcare provider.
Recovery and Outcome
How long after blastocyst transfer is implantation?
After undergoing a blastocyst transfer, many couples might wonder how long it will take for implantation to occur. It's important to keep in mind that the timeline can differ from person to person and pregnancy rates can vary.
- Typically, implantation occurs between 6-10 days after the blastocyst transfer. However, some patients may experience implantation earlier or later than this timeframe.
- During this period of time, it's crucial for individuals who have undergone a blastocyst transfer to continue following their doctor's orders regarding medications and activity levels as any disruption could potentially hinder successful implantation.
- It is also essential not to jump to conclusions too early during the two-week wait as signs of pregnancy such as spotting or cramping may be misleading and not necessarily indicative of successful implantation.
- While there are general guidelines on how long after a blastocyst transfer an embryo implants, it’s vital for each individual patient to consult with their fertility specialist about their unique situation.
Key Takeaway:
- Blastocyst transfer is a technique of in vitro fertilization (IVF) that involves transferring embryos to the uterus at a later stage of development, which may increase the chances of successful implantation and pregnancy.
- The term 'blastocyst' refers to an embryo that has developed over several days and contains about 100 cells.
- Blastocysts have two distinct parts: the inner cell mass, which will eventually become the fetus, and the outer layer of cells called trophoblasts which will form into the placenta.
- Blastocyst transfer has risks and disadvantages, including multiple pregnancies and emotional stress, but remains an effective option for many individuals struggling with infertility who wish to pursue parenthood through assisted reproductive technology.
- Success rates depend on several factors, including the age and health of the woman and the quality of the embryos.
Frequently asked questions:
- What is the success rate of blastocyst transfer?
62% - How long after a blastocyst transfer can you get pregnant?
- What day of cycle is blastocyst transfer?
Day 5
Reference
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2593763/#:~:text=Blastocyst%20transfer%20has%20a%20higher,double%20embryo%20transfer%20%5B13%5D.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2700692/
- https://pubmed.ncbi.nlm.nih.gov/9457938/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5672726/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7812106/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8139971/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8083859/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2441538/
- https://pubmed.ncbi.nlm.nih.gov/2612378/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2846056/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7074270/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2700692/

Dr Purva Singh
MBBS MS OBGYNIVF Specialist